To process an invoice using Online Patient Claiming:
Ensure you have created invoices to send to Medicare.
Open the Practice Explorer and select Medicare Australia from the Margin menu. The Medicare Australia Online Claims window appears.

Multiple claims can be selected and processed together by highlighting the required claims. The claims can also be sorted to group like claims before selecting them.
Right-click the list of payee rooms to allow selection/de-selection of all rooms.
To edit an existing claim, select the Claim and click  . Edit the claim details and transmit as required.
. Edit the claim details and transmit as required.
To delete an existing claim, select the Claim and click Delete
The claim must be deleted on the same day which it was submitted;
-
Medicare must be notified by phone that the claim is to be deleted;
-
A reason for the deletion must be entered (allows for space up to 128 characters);
-
The user must confirm that they have contacted Medicare to delete the claim;
-
Should Medicare provide some reference for the deletion, this should be entered in the reason text for future reference.
-
Once the claim has been deleted, invoices attached to the claim will be available for selection with new claims;
-
No transmission is involved with the deletion process;
-
Unlike deleting an un-submitted claim, all "same day deleted" claims will remain viewable in the claims list.
Click New to begin a new batch of claims. The New Medicare Online Claim window appears.
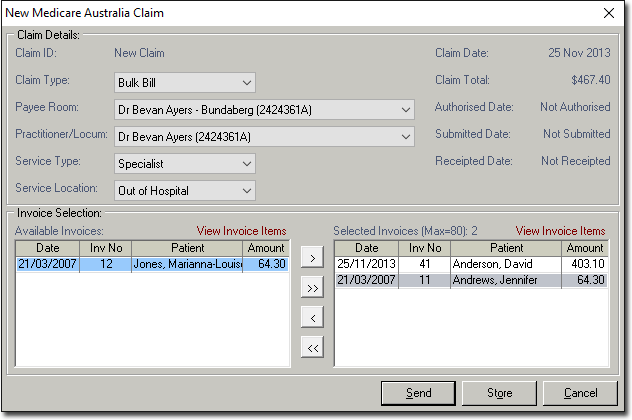
Select the Claim Type, Payee Room, Practitioner, Service Type, and Service Location for the claim.
If in General Practitioner settings you have indicated that the practitioner has only one Service Type, the Service Type drop-down menu here will default to the corresponding Type. On the other hand, if the practitioner has multiple Service Types there will be no default selected here, and you must manually select one.
The available invoices that meet these criteria, are displayed in the lower section of the window.
To view details of an invoice select the invoice and click View Invoice Items (located on the top right hand corner of the Available Invoices and Selected Invoices sections).
Select the > or < buttons to move selected invoices into and out of the claim. Select the >> or << buttons to move all invoices into and out of the claim.
Claims may be selected by dragging and dropping the invoice with the mouse. Resubmitted invoices are displayed in red text. A maximum of 80 claims can be batched simultaneously.
Click  to authorise, but not immediately transmit the claim, or click
to authorise, but not immediately transmit the claim, or click  to send the items to Medicare. The Medicare Online Claim Authorisation window appears.
to send the items to Medicare. The Medicare Online Claim Authorisation window appears.
The authorisation required will depend on how you have setup Bluechip and your agreement with Medicare.

Click OK. to send the transaction. The Medicare Australia - Authorising Claim window appears.
Click  once the processing has completed. You are returned to the Medicare Online Claims window.
once the processing has completed. You are returned to the Medicare Online Claims window.
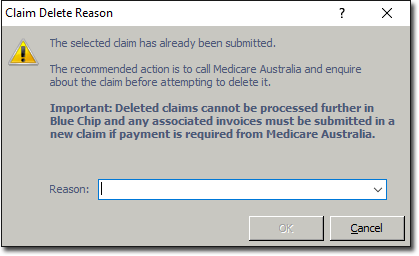
Select a claim to delete if required and click Delete The Claim Delete Reason window appears. For more information on deleting claims refer to Claim Delete Reason window.
The Claim Delete Reason window only displays when deleting a claim that was submitted on the same date as the deletion. Claims submitted on prior dates can not be deleted. If deleting a claim that has been authorised, but not submitted, a standard yes/no prompt is displayed.
The practice MUST contact Medicare and arrange the same-day deletion, before deleting the claim in Bluechip. To facilitate this, the OK button remains disabled until the user selects the box that confirms they have contacted Medicare.
*sample image
Click  to view the Transmission log for the selected claim. The Medicare Online Claim Transmission Log is displayed.
to view the Transmission log for the selected claim. The Medicare Online Claim Transmission Log is displayed.

Click  to view items rejected by Medicare during processing of the selected claim. The Medicare Australia Claim Rejected Items window appears.
to view items rejected by Medicare during processing of the selected claim. The Medicare Australia Claim Rejected Items window appears.

Select the option suitable to your practice accounting methods and click OK. to resolve the item.
Items that are not fully paid may be written off or left unpaid and referred to the patient for payment (based on your practice procedures). Items that are over paid will result in a Sundry Invoice being created to which the residual funds are allocated. Sundry payments made by Medicare can also be receipted.
Items that have been are rejected, and for which no amount has been paid, may be resubmitted. The resubmission process involves Bluechip writing off the original invoice, copying it, attaching the copied invoice item to a new invoice and entering service text for the invoice item to allow the claim to be referred to the Medicare Officer for consideration.
You must attach the new invoice to a new claim and submit it to Medicare for payment.
Click  to receipt items returned from Medicare. The Medicare Australia Claim Receipt window appears. For items not paid in full, select the option suitable to your practice accounting methods and click OK. to receipt the item.
to receipt items returned from Medicare. The Medicare Australia Claim Receipt window appears. For items not paid in full, select the option suitable to your practice accounting methods and click OK. to receipt the item.

Click  to update patient information with details returned from Medicare. The Patient Updates window appears.
to update patient information with details returned from Medicare. The Patient Updates window appears.
When submitted patient information differs form that held by Medicare, corrected patient information is returned with the processing report. This information can then be used to update the Bluechip record for the patient using the Updates button.

Select the appropriate option for each patient record, or click  or
or button.
button.
Click OK. The patients records are updated with the relevant information from Medicare.
Notes on Sending Invoices to Medicare Online
There can be a maximum of 80 vouchers per claim.
There can only be a maximum of 14 invoices per voucher.
The Claim ID is set automatically by Bluechip and cannot be changed. The Claim ID follows the format xnnnn@ where:
x is and alpha (except I or O) or # for in-hospital services (Note: the # is not used for DVA claims unless one of the vouchers in the claim has an "Hospital" referral type. If this is not the case, the letter A is used).
nnnn is a four(4) digit number. Should this number exceed 9999, it will be reset to 0.
@ identifies the claim as an electronic claim for Medicare Online.
Medicare has 3 main statuses for a claim item:
Paid
Accepted as Referred to a Medicare Operator
Rejected
Processing and payment reports will not be available until Medicare has assessed all items in the claim.
All vouchers in a claim must be for the same servicing provider and same payee provider.
All vouchers must be authorised before they can be sent.
The hospital name must be sent to Medicare for all services which are "in hospital".
Invoices cannot be created for a Medicare Online batching account if the eligibility check is not passed.
A claim cannot be edited or deleted once transmitted to Medicare.
The servicing provider can only be a locum or the payee provider. Only one servicing provider can be nominated per claim. If a Practitioner in the practice (that is a Practitioner associated with a room) is providing a service for another Practitioner, they must set themselves up as a locum. This requirement is to prevent bank transfer entry problems. The transfer of moneys between the Practitioners involved in these circumstances must be handled outside of Bluechip.
Only invoices which are for an account associated with the payee provider (room) and for the nominated practitioner can appear in the available invoices list.
The list of servicing providers is assembled from the Practitioner and locums that have raised invoices for the nominated payee provider room.
To appear in the available invoices list, invoices must:
Have no allocations against them.
Not be attached to another claim (excluding those claims that are same day deleted).
Have a balance greater than zero.
Not be adjusted.
Not be associated with a deleted patient.
Have an issue date less than or equal to the current date.
Store and Forward Method – When using the store and forward method, the claim record is saved and can be transmitted at a later time from the Medicare Online Claims window.
Authorising and/or sending a claim will invoke the Medicare Online - Processing Claim(s) window as described in Transmitting.
The processing window will close automatically once processing has completed successfully. If an error occurs during processing, the window will remain open to allow for the errors to be reviewed and the processing information saved to file as desired.
An authorised claim can be edited provided that it has not been submitted.