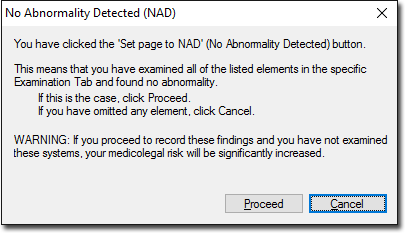
The History module of Progress Notes allows you to record data regarding the patient's clinical history. Each tab within the History module contains a variety of controls for recording information, as shown in the following image. Information recorded using any of the tools within the History module appears in the text box at the upper-left of the window, and upon saving is added to the Progress Notes for the consultation.
It is important that you don't confuse this History module within Progress Notes with the Past History tab from the patient's record. The former is used to record symptoms that have become evident since the patient's last consultation, whereas the latter is used to record conditions that the patient has/had. Furthermore, data recorded using the History module is saved within the current Progress Note, and is valid only for that Progress Note, and has no bearing on any other modules or functionality within MedicalDirector Clinical. On the other hand, data recorded using the Past History tab is used in functionality such as drug interaction checking and immunisation checking.
The content available to this module differs depending on the patient's recorded sex at birth.
Available Tabs
|
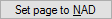
Allows you to set all options on the current tab to 'No Abnormalities Detected'. Upon clicking this, you will be prompted with the following:
|
|
Clear all data you have recorded for the current tab. |
|
Opens the Progress Notes Examination module. |