Progress Notes is the component of the patient's record in which you record notes about their visit to the Practice; their reason for visiting, examinations performed on them, medications you prescribed on the day, and so on. To manage a patient's Progress Notes, select the Progress tab in the Clinical Window .
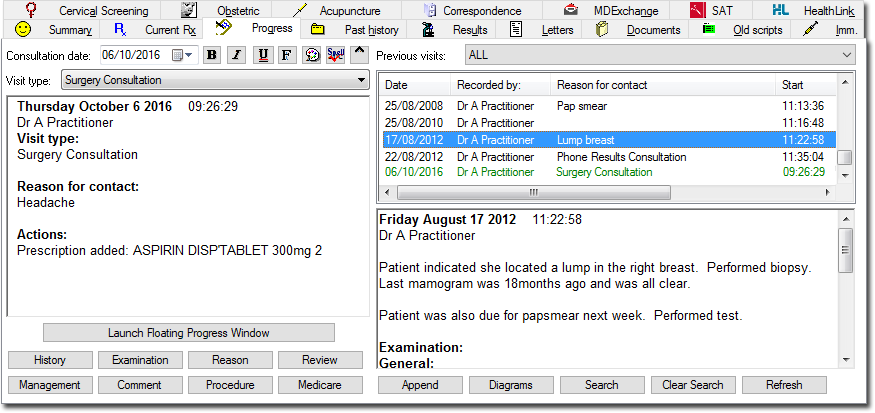
The Progress Notes display is divided into two sections;
The left-hand panel is where notes are recorded. Text can be typed directly in this area, and can be formatted by altering font, colour and appearance (bold, italics and underline) if required.
Many notes are recorded here automatically by Clinical as you use its various tools, and notes are automatically saved when you leave a patient's record (provided this option is enabled).
This area can be viewed as a mini, floating window that can be relocated and resized. This is also available via Patient > Floating Progress Tab.
The right-hand (split) panel displays a history of Progress Notes.
The upper-half lists past Progress Notes in order of visit, with the lower-half showing the detail of any selected past Progress Note.
This list also displays the current Progress Note (the Note you are actively working on), highlighted in green.
When you open the patient's record, the latest recorded Note is selected by default.
During a consultation it is possible that newer Notes appear in this list periodically, placed after the Note you are currently working on. This is because it is possible for multiple users to work on the same patient's record simultaneously i.e. another user may save a Note whilst you are still working on yours.
Considerations:
If no notes have been recorded and no actions performed whilst in the patient's Progress Notes, you will be prompted as to whether to save a record of their visit. Upon closing a patient's record, the elapsed time the notes were open, as well as the start and finish times are recorded in the database.
Progress Notes are automatically saved at the end of the visit.
Each user can write a unique Progress Note (even in restricted mode).
You can modify your last Note (created today) up until midnight.
In restricted-mode, most features on the Progress tab are disabled. However you can write notes, and access Comments/Management.
You can resume your previous note (created today), provided you don’t already have it open on another computer.
Consultation Date |
Allows you to select the date of consultation before you enter any notes. This is useful if for example you saw a patient last week, but forgot to enter any notes for that visit; by selecting the day on which their consultation took place, you can record notes for that day with the assurance that when saved, the notes will be listed correctly in order of visit-date, not recording-date. |
Previous Visits |
This drop-down menu allows you to filter the display of previous visits according to Reason for Contact. |
Current Visit Box |
This large text box to the left of the Progress window is where Progress Notes for the current visit are recorded and displayed. Whilst it is possible to type text directly into this box, other notes are added automatically as a result of using the various components of Clinical. For example, printing a prescription generates an entry. Also the current date, time and practitioner name is entered by default for new notes. |
|
Add any notes to the patients previous visits. |
|
Clear the search criteria. |
|
Enable user-defined blocks of text to be inserted at the current cursor position. A number of text blocks can be stored for each practitioner. |
|
View any diagrams recorded during previous visits for the patient. Diagrams are entered through the Examination window. The Diagrams button is disabled if no diagrams have been recorded. |
|
Record examination findings using a combination of Yes/No controls, Check boxes, spin boxes, and Pick lists. Some areas enable you to draw on diagrams of sections of the body. |
|
Launches a mini, floating version of the Progress Notes window that can be relocated and resized. This is also available via Patient > Floating Progress Tab.
|
|
Display a series of tabbed pages to allow entry of an historical review. Each major system has its own page containing buttons and lists to enable the entry of symptoms without having to type. |
|
Add Management text. Management items are 'frequently-used text that inserted using a shortcut key combination.' |
|
Associate a Medicare item number with a visit. |
|
Enter the details of any procedure performed on the patient into a Procedure section of the notes. It uses part of the DOCLE coded list that is also used elsewhere in Clinical. See also the Diagnosis Coder. |
|
Enter a reason for the patient's visit/contact. See also the Diagnosis Coder. |
|
Review a date or interval to be recorded in the notes. |
|
Search the patient's previous progress notes for specified text entries. Clear the search. |
|
Refreshes the list of previous visits. If multiple users have the same patient's record open simultaneously, clicking this button will refresh your list to display any past notes saved by other users during this session. |
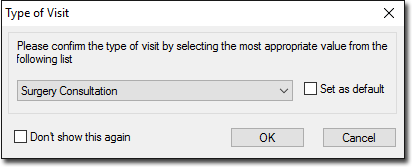
From the Visit Type list you can indicate the type of visit for the day’s consultation. The default visit type for practitioners is ‘Surgery Consultation’, and the default for all other users is 'Practice Admin'. You can add customised entries via the Lists tab of Clinical Options. You can set the default via the Progress Notes tab of Clinical Options.
Your selected Visit Type for each consultation is also displayed in the past Progress Notes.
Upon closing the patient’s record, you will be prompted to confirm the visit type you have selected.
Both the drop-down list on the Progress Tab and the associated prompt can be disabled via Progress Notes options. |
Progress Notes Shortcut Keys - see also Keyboard Shortcuts |
|
S: |
Subjective |
O: |
Objective |
A: |
Assessment |
P: |
Plan |
Hx |
History |
OE |
Examination |
Dx |
Reason for contact |
Mx |
Management |